Renal failure, otherwise known as kidney failure, is a medical condition whereby the kidneys are no longer able to perform their functions properly.
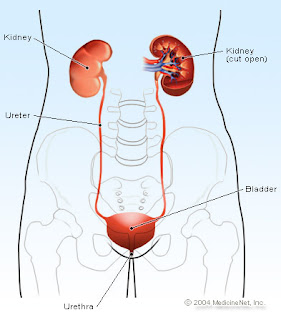
Kidneys are vital to our health as they regulate the removal of metabolic waste products from our bodies. Waste products in different parts of our bodies are extracted by the kidneys into the bloodstream. These waste products then travel through the ureter to the bladder and are excreted from our bodies through urine.
Failure of the kidneys to carry out their role will result in the accumulation of metabolic waste in our bodies due to insufficient filtration of the blood. This results in abnormally high levels of nitrogen-containing compounds, such as urea, creatinine, various body waste compounds and other nitrogen-rich compounds in the blood. This build-up is termed as azotemia. Mild azotemia may show little or no symptoms. However, if renal failure continues to deteriorate, symptoms will start to develop and lead to a severe condition termed as uremia.
Renal function can be measured by the glomerular filtration rate (GFR). However, in clinical practice, creatinine clearance or estimates of creatinine clearance based on the serum creatinine levels are used to measure GFR. Creatinine is a break-down product of creatine phosphate in muscles.
We are actually able to survive with a single healthy kidney since the amount of renal tissue in one kidney is more than necessary to maintain homeostatic functions and keep us alive. However, when there is a great decrease in the amount of functioning renal tissues, renal failure occurs.
Renal failure is generally divided into 2 types:
Kidneys are vital to our health as they regulate the removal of metabolic waste products from our bodies. Waste products in different parts of our bodies are extracted by the kidneys into the bloodstream. These waste products then travel through the ureter to the bladder and are excreted from our bodies through urine.
Failure of the kidneys to carry out their role will result in the accumulation of metabolic waste in our bodies due to insufficient filtration of the blood. This results in abnormally high levels of nitrogen-containing compounds, such as urea, creatinine, various body waste compounds and other nitrogen-rich compounds in the blood. This build-up is termed as azotemia. Mild azotemia may show little or no symptoms. However, if renal failure continues to deteriorate, symptoms will start to develop and lead to a severe condition termed as uremia.
Renal function can be measured by the glomerular filtration rate (GFR). However, in clinical practice, creatinine clearance or estimates of creatinine clearance based on the serum creatinine levels are used to measure GFR. Creatinine is a break-down product of creatine phosphate in muscles.
We are actually able to survive with a single healthy kidney since the amount of renal tissue in one kidney is more than necessary to maintain homeostatic functions and keep us alive. However, when there is a great decrease in the amount of functioning renal tissues, renal failure occurs.
Renal failure is generally divided into 2 types:
- Acute Kidney Injury (AKI)
- Chronic Kidney Disease (CKD)








.jpg)







